Hashimoto’s disease, also known as Hashimoto’s thyroiditis, is the most common type of chronic lymphocytic thyroiditis in humans. This autoimmune disorder was first discovered by a Japanese physician named Hakaru Hashimoto in 1912, and the disease is named after him.
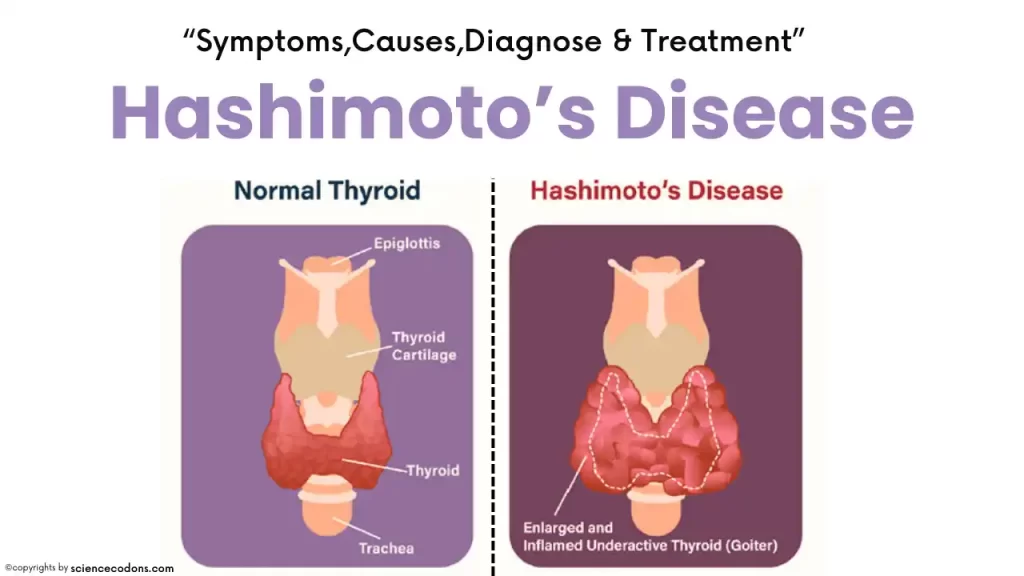
The thyroid gland is one of the most crucial endocrine glands in the body. It is located in the front of the neck, resembling two butterfly wings on the tracheal cartilage. The primary function of the thyroid gland is to produce thyroid hormones, which regulate the body’s metabolic processes—converting ingested food into energy. Additionally, thyroid hormones play a vital role in the growth and development of the central nervous system in infants and children. The term thyroiditis refers to inflammation of the thyroid gland, which can result from either an infection of the gland or an autoimmune phenomenon.
In Hashimoto’s disease, abnormal substances called antibodies or autoantibodies are secreted into the bloodstream by the immune system, targeting the thyroid gland. Specifically, these autoantibodies, known as anti-thyroid peroxidase antibodies (TPO antibodies), primarily attack an essential enzyme involved in the synthesis of thyroid hormones—the enzyme called thyroid peroxidase. As a result, the function of the thyroid gland gradually becomes impaired, leading to hypothyroidism (underactive thyroid).
Risk factors for Hashimoto’s disease include:
Lymphocyte infiltration in the thyroid gland can cause destruction and fibrosis of its tissue. The exact underlying cause of the immune response remains unknown. Still, it may be associated with other autoimmune conditions such as type 1 diabetes, celiac disease, lupus, and other immune-related disorders. Both genetic and environmental factors play a role in its development. Excessive iodine intake, selenium deficiency, and certain infectious diseases are among the recognized environmental factors.
- Gender: Hashimoto’s disease affects women more frequently. Researchers believe that sex hormones play a significant role in this susceptibility.
- Age: The likelihood of developing Hashimoto’s disease increases with age. Women, individuals with a family history of the disease, and anyone with an autoimmune condition are at higher risk.
- Menopause: Reduced estrogen levels during menopause may impact thyroid function.
Symptoms of Hashimoto’s disease
It is more common in individuals aged 30 to 50, and women are more frequently affected than men. In the early stages, patients often exhibit minimal symptoms, except for a slight feeling of pressure in the neck and fatigue. Initially, a firm and slightly irregular goiter (enlarged thyroid gland) may form, gradually increasing in size. In about 10% of cases, there may be accompanying pain. As hypothyroidism progresses, clinical signs and symptoms become more evident. These include:
- Fatigue
- Depression
- Weight gain
- Cold intolerance
- Sleepiness
- Dry and brittle hair
- Constipation
- Dry skin
- Hoarseness
- Reduced concentration
- Vague body pains
- Facial puffiness and swelling
- Menstrual irregularities in women
- Swelling of the legs
What are the warning signs of Hashimoto’s?
Severe hypothyroidism can lead to complications such as periorbital edema (swelling around the eyes), reduced heart rate, lower body temperature, and even life-threatening myxedema coma. Untreated hypothyroidism may cause cardiac enlargement, worsening heart failure, and accumulation of fluid around the lungs (pleural effusion) or heart (pericardial effusion).
Other signs and symptoms include:
- Thyroid gland swelling (due to inflammation) can cause discomfort or pressure in the throat.
- Goiter, an enlarged thyroid gland in the front of the neck.
- Difficulty swallowing solid foods or liquids due to thyroid gland enlargement and pressure on the esophagus.
| Symptoms | Descriptions |
|---|---|
| Fatigue and sluggishness | Feeling tired and lacking energy. |
| Increased sensitivity to cold | Feeling excessively cold even in normal temperatures. |
| Increased sleepiness | Experiencing excessive sleepiness or drowsiness. |
| Dry skin | Skin becomes dry, flaky, and lacks moisture. |
| Constipation | Difficulty passing stools or infrequent bowel movements. |
| Muscle weakness | Reduced strength and ability to perform physical tasks. |
| Muscle aches, tenderness, and stiffness | Pain, soreness, and stiffness in muscles. |
| Joint pain and stiffness | Discomfort and limited movement in joints. |
| Irregular or excessive menstrual bleeding | Abnormal or heavy menstrual periods in women. |
| Depression | Persistent feelings of sadness, hopelessness, or low mood. |
| Problems with memory or concentration | Difficulty focusing, remembering, or thinking clearly. |
| Swelling of the thyroid (goiter) | Enlargement of the thyroid gland in the neck. |
| A puffy face | Facial swelling, especially around the eyes. |
| Brittle nails | Nails become weak, break easily, or show ridges. |
| Hair loss | Thinning hair or hair falling out. |
| Enlargement of the tongue | The tongue may become larger than usual. |
Hashimoto’s thyroiditis diagnosis(Methods)
Here are the key points regarding its diagnosis and evaluation:
Clinical Assessment:
- The physician evaluates common symptoms and complaints associated with hypothyroidism.
- The neck is examined for thyroid gland enlargement.
- Detailed family history is obtained.
Blood Tests
- Thyroid function tests (TFTs) are essential.
- Initially, thyroid hormone levels (T3 and T4) may appear normal.
- As hypothyroidism progresses, thyroid hormone levels decrease, and thyroid-stimulating hormone (TSH) levels rise.
- TSH measurement in blood is the most useful method for assessing thyroid status.
Anti-Thyroid Peroxidase Antibodies (Anti-TPO):
- These antibodies are involved in thyroid hormone production.
- Elevated levels of anti-TPO antibodies indicate Hashimoto’s disease.
- Even in the early stages, patients may have increased TSH levels, even within the normal range of thyroid hormones.
- The gold standard test for Hashimoto’s thyroiditis
Ultrasound of the Thyroid:
- It is helpful in assessing thyroiditis and gland size.
Treatment of hypothyroidism
The primary treatment for Hashimoto’s disease involves a synthetic thyroid hormone called levothyroxine.
Levothyroxine
This medication restores normal thyroid function and is typically taken orally. Patients need to take it daily throughout their lives. Levothyroxine not only provides the necessary thyroid hormone but also helps reduce the size of the goiter (enlarged thyroid gland) by suppressing the production of thyroid-stimulating hormone (TSH) from the pituitary gland. In many patients, the goiter may shrink after 6 to 18 months. Regular follow-up with a treating physician is essential to adjust the medication dosage as needed.
Surgery
Since hypothyroidism and Hashimoto’s disease can be managed with medications, surgical removal of the thyroid gland is usually unnecessary. However, in cases where a patient has a significantly enlarged goiter that doesn’t change in size despite thyroid medication, surgery may be considered for cosmetic reasons or to relieve pressure on nearby structures such as the trachea and esophagus.
Foods & supplements(recommended diet)
Regarding dietary recommendations, there is no specific diet for Hashimoto’s disease, and there is no evidence supporting the impact of specific foods on worsening or improving the condition. However, some foods, medications, or supplements may affect an individual’s ability to absorb prescribed levothyroxine. For instance:
- Iron and calcium supplements: Taking these supplements within four hours of levothyroxine may help prevent interference.
- Medications for stomach ulcers: Certain medications, such as antacids or proton pump inhibitors (e.g., omeprazole), can affect levothyroxine absorption.
- Selenium-rich foods: Consuming foods rich in selenium (e.g., sunflower seeds, Brazil nuts) may support thyroid health.
Additionally, maintaining a healthy lifestyle, regular exercise, good sleep, stress management, and a balanced diet can contribute to overall well-being and potentially reduce the risk of developing Hashimoto’s disease.
Note! Untreated hypothyroidism during pregnancy may increase the risk of miscarriage, premature birth, or stillbirth, and it could potentially lead to dangerous hypertension in late pregnancy (known as preeclampsia). Additionally, untreated hypothyroidism can impact the physical growth and brain development of the child.
Conclusion
Hashimoto’s disease is a chronic autoimmune disorder that affects the thyroid gland, a small organ at the base of the neck that produces hormones that regulate the body’s metabolism. In Hashimoto’s disease, the immune system mistakenly attacks the thyroid cells, causing inflammation and damage. This leads to reduced thyroid function and low levels of thyroid hormones, a condition known as hypothyroidism. Hashimoto’s disease is the most frequent cause of hypothyroidism in the United States and other countries where iodine intake is adequate. The treatment of Hashimoto’s disease involves taking thyroid hormone replacement therapy, which restores normal thyroid function and relieves the symptoms of hypothyroidism. The management of Hashimoto’s disease also involves adopting a healthy lifestyle and addressing any complications or associated conditions. Following these steps can improve your quality of life and well-being.
Reference:
- The American Thyroid Association
- Hashimoto’s Thyroiditis: Lifestyle Interventions for Finding and Treating the Root Cause by Izabella Wentz, PharmD
- Root Cause by Amy Myers, MD