Congenital hypothyroidism (CH) is a condition that affects newborn babies who are born with low or no thyroid hormone. Thyroid hormone is essential for normal growth and development of the brain and body.
The natural development and maturation of the fetal thyroid gland and the production of thyroid hormones play a vital role in brain development during fetal life and beyond. In the first half of pregnancy, thyroid hormone concentrations in the fetal bloodstream are low. During this period, the fetus relies entirely on maternal thyroid hormones, which cross the placenta to reach the developing baby. Key milestones include the production of thyroglobulin around weeks 4 to 6, iodine retention between weeks 8 to 10, and the initiation of thyroid hormone production (primarily thyroxine and, to a lesser extent, triiodothyronine) in the fetal thyroid gland around week 12 of pregnancy.
The precise clinical manifestations of severe thyroid deficiency, known as cretinism, were first described by Sir William Osler in 1897. Although thyroid extract was effective in alleviating the physical symptoms of congenital hypothyroidism, irreversible mental retardation often occurred due to delayed diagnosis and treatment initiation after a critical period of brain growth and development.
Fortunately, with the implementation of newborn screening programs for congenital hypothyroidism, early identification, and immediate treatment have helped control mental retardation resulting from this condition.
Prevalence of congenital hypothyroidism
The prevalence of congenital hypothyroidism varies worldwide. Before the era of widespread universal screening, the estimated occurrence was approximately one case per 5,000 to 10,000 births.
The first congenital hypothyroidism screening program began in 1974 in Quebec, Canada. In the initial report, which screened 175,000 infants, the disease’s incidence was roughly one case per 6,000 births. With the expansion of screening programs in industrialized countries, Eastern Europe, South America, Asia, and Africa, millions of newborns are now screened annually for congenital hypothyroidism.
The prevalence of congenital hypothyroidism varies across different countries due to factors such as maternal iodine intake, racial differences, genetic factors, and screening methods. Generally, the prevalence of congenital hypothyroidism in a region is closely and directly related to the iodine supply in that area. Specifically, reported rates of congenital hypothyroidism include one case per 3,500 to 5,000 births in the United States, one case per 3,000 births in Europe, one case per 6,600 to 7,300 births in Sweden, and one case per 5,700 births in Japan. Notably, the prevalence of this condition is higher among individuals of Asian descent, and in Greece, it has been reported as one case per 800 live births.
- In the United States, it affects approximately 1 in 3500 to 5000 newborns.
- In Europe, the incidence is around 1 in 3000 births.
- In Sweden, it occurs in 1 in 6600 to 7300 births.
- In Japan, the reported incidence is 1 in 5700 births.
- Generally, the prevalence is higher among individuals of Asian descent.
- In Greece, it is reported in 1 in 800 live births
Prevalence of CH in Iran
In 1993, simultaneous with the start of the universal iodine supplementation program, a similar study was conducted in Shiraz and five neighboring cities. In this study, the incidence rate of congenital hypothyroidism was found to be one case per 1433 live births.
With increased iodine consumption by Iranian households and the correction of iodine deficiency in the community, there was a need to restart the congenital hypothyroidism screening program. The first phase of this project was implemented in 1997, covering five government hospitals affiliated with Shahid Beheshti University of Medical Sciences. Over a period of 14 months, approximately 3000 newborns underwent screening, leading to the detection of 3 cases of congenital hypothyroidism. Overall, based on initial screening studies in Tehran, Shiraz, and Isfahan, the estimated average incidence of congenital hypothyroidism in the country is one case per 1000 live births.
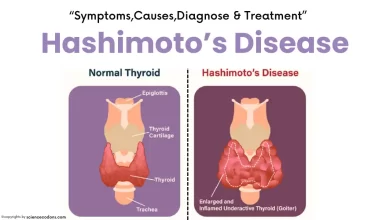
What Causes congenital hypothyroidism?
CH can be caused by different factors that affect the development or function of the thyroid gland, which is a butterfly-shaped organ in the neck that produces thyroid hormone. The most common causes of CH are:
Thyroid dysgenesis: This means that the thyroid gland is absent, underdeveloped, or abnormally located. This accounts for about 85% of CH cases and is usually permanent.
Thyroid dyshormonogenesis: This means that the thyroid gland is present but cannot make enough thyroid hormone because of a defect in the hormone synthesis pathway. This accounts for about 10% to 15% of CH cases and can be permanent or transient.
Iodine deficiency: This means that the mother or the baby does not get enough iodine, which is a mineral that is needed for thyroid hormone production. This is a common cause of CH in some parts of the world where iodine intake is low, but rare in developed countries where iodized salt is widely used2.
Maternal factors: This means that the mother has a condition or takes a medication that affects the baby’s thyroid function. For example, some mothers have antibodies that block or destroy the baby’s thyroid gland or take antithyroid drugs that cross the placenta and inhibit the baby’s thyroid hormone production
Types of congenital hypothyroidism
During fetal development, the thyroid hormones play a crucial role in the growth and evolution of all body organs, especially the central nervous system. This role begins around the 11th week of gestation and continues throughout the period of physical, physiological, and psychological growth and maturity.
The deficiency of thyroid hormones during fetal life and the first year after birth is often associated with a wide range of neuropsychological disorders. These disorders can manifest as developmental delays, macrocephaly (enlarged head), open posterior fontanelle, jaundice, and delayed skeletal system development.
The classification of congenital hypothyroidism can be divided into three types:
- Primary Hypothyroidism: This type results from a disorder within the thyroid gland itself.
- Secondary Hypothyroidism: It occurs due to an abnormality in the pituitary gland (hypophysis).
- Tertiary Hypothyroidism: This rare form originates from a disorder in the hypothalamus or the thalamus.
Congenital hypothyroidism can be transient (temporary) or permanent. The primary and permanent forms are the most common among newborns and represent the most prevalent endocrine disorder at birth. Approximately 80% to 90% of cases of permanent congenital hypothyroidism result from isolated developmental disorders of the thyroid gland, known as thyroid dysgenesis. This term encompasses complete absence or incomplete formation of the thyroid gland, including ectopic thyroid tissue.
About 10% to 20% of cases are due to defects in thyroid hormone production (dyshormogenesis), which can occur at any stage of hormone synthesis, from iodine transport to thyroglobulin formation. These disorders are often inherited and have a higher prevalence in consanguineous marriages.
Permanent central hypothyroidism (originating from the hypothalamus or pituitary gland) is extremely rare and typically affects only one in 50,000 newborns. In this type, there is always concurrent deficiency of other pituitary or hypothalamic hormones.
Congenital hypothyroidism symptoms
Clinical manifestations of congenital hypothyroidism may vary. Some infants may show no signs at all, while others might exhibit mild effects that often go unrecognized. However, severe cases can lead to permanent growth failure and intellectual disability. Here are some common clinical signs and symptoms:
- Delayed Birth: Some affected newborns may experience delayed birth.
- Macrocephaly: Enlargement of the head (macrocephaly) can occur.
- Posterior Fontanelle: The posterior fontanelle (soft spot on the back of the head) may remain open.
- Jaundice: Prolonged jaundice can be observed.
- Skeletal System Delay: Delayed skeletal system development may occur.
- Goiter: A small percentage of newborns may have an enlarged thyroid gland (goiter).
Other signs and symptoms include:
- feeding difficulties
- hypothermia
- lethargy
- constipation
- prolonged neonatal jaundice
- abdominal distension
- umbilical hernia, dry skin
- large tongue
- hoarse cry
- puffy appearance
In case of clinical suspicion of congenital hypothyroidism in newborns, TSH and free thyroxine measurements are performed immediately, even if the newborn has been screened at birth, and the newborn is treated with thyroid tablets until the result is ready. Newborns with central type of congenital hypothyroidism are usually affected by low blood sugar or hypoglycemia or small genitalia (micropenis) and undescended testicles. The presence of developmental disorders such as cleft palate or cleft lip and optic nerve hypoplasia may also indicate a disorder in the pituitary gland.
| Symptom | Description |
|---|---|
| Weak cry | Babies may have a feeble or weak cry. |
| Poor feeding | Difficulties with feeding or inadequate feeding. |
| Constipation | Infrequent bowel movements or difficulty passing stool. |
| Dry skin | The skin may appear dry and flaky. |
| Poor muscle tone | Babies may exhibit floppiness or poor muscle strength. |
| Cold hands and feet | Extremities (hands and feet) may feel cold and appear mottled. |
| Prolonged jaundice | Yellowing of the skin that persists beyond the usual timeframe after birth. |
How Is CH Diagnosed?
CH is usually diagnosed by newborn screening (NBS), which is a blood test that is done for all babies shortly after birth. NBS measures the level of thyroid-stimulating hormone (TSH) in the baby’s blood. TSH is a hormone that stimulates the thyroid gland to make thyroid hormone. If the thyroid gland is not working properly, the TSH level will be high, indicating CH. NBS can also measure the level of free thyroxine (FT4), which is the main form of thyroid hormone in the blood. If the FT4 level is low, it also indicates CH4.
If NBS shows abnormal results, the baby will need further testing to confirm the diagnosis and find the cause of CH. These tests may include:
- Repeat blood tests
- Thyroid scan
- Thyroid ultrasound
- Genetic testing
Treatment of congenital hypothyroidism
Treatment of congenital hypothyroidism in all newborns involves promptly prescribing thyroid hormone to ensure that their blood thyroid hormone levels fall within the normal range. The goal of natural treatment is to normalize serum thyroxine (T4) levels within 2 weeks and thyroid-stimulating hormone (TSH) levels within 1 month.
The initial dose of levothyroxine is 10 to 15 micrograms per kilogram of the newborn’s weight. The powdered tablet is dissolved in water or breast milk and administered to the infant. Simultaneous use of iron compounds and dietary supplements with levothyroxine should be avoided.
If higher doses are used (12 to 17 micrograms per kilogram of weight), serum thyroxine levels reach therapeutic targets within 3 days and TSH levels within 2 weeks. The appropriate increase in serum thyroxine can be evaluated by measuring free serum thyroxine one week after starting treatment. Throughout the first 3 years of treatment, total and free serum thyroxine levels should be maintained above the upper limit of the normal range, while TSH levels should remain within the lower normal range.
Follow-up for Congenital Hypothyroidism in Newborns
Clinical examinations should be conducted every few months, including growth and development assessments during the first 3 years of treatment. Newborns with congenital hypothyroidism are at risk of developing congenital abnormalities (approximately 10% compared to 3% in healthy newborns). The most common cardiovascular abnormalities include pulmonary artery stenosis and atrial or ventricular septal defects.
During follow-up, serum thyroxine (T4) and thyroid-stimulating hormone (TSH) levels are measured as follows:
- Week 2 and 4 after treatment initiation
- Then, at intervals of 1 to 2 months during the first 6 months of life
- Every 3 to 4 months from 6 months to 3 years of age
- Every 6 to 12 months until complete growth
- 4 weeks after any dose adjustment of levothyroxine
Despite the importance of timely treatment and continuous management of congenital hypothyroidism, there are reports even from advanced countries indicating shortcomings in the care and treatment of affected infants and children. The consequences may include reduced intelligence quotient (IQ) and varying degrees of mental retardation, especially during adolescence and young adulthood. To prevent complications and ensure proper treatment for these patients, parental education on the care and follow-up of their children is essential.
Conclusion
CH is a condition that affects newborn babies who are born with low or no thyroid hormone. It can cause serious problems such as intellectual disability, growth failure, and other health issues if not detected and treated early. NBS can help diagnose CH in the first days of life, and L-T4 can help treat CH and prevent complications. With proper treatment and follow-up, most babies with CH can lead normal and healthy lives.
Reference:
- Nelson Textbook of Pediatrics, 21st Edition – Chapter 158: Congenital Hypothyroidism
- American Thyroid Association: Congenital Hypothyroidism
- Medscape: Congenital Hypothyroidism: Practice Essentials, Background, Pathophysiology
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9610765/
- https://www.ijpediatrics.com/index.php/ijcp/article/view/5673