Individuals aged 65 and older are considered elderly. Approximately 6 million people, which accounts for 4.6% of Iran’s population of 83 million, fall into the age group above 65, and about 5.8 million individuals (approximately 9.9%) are over 60 years old.
As individuals age, several changes occur in the thyroid gland
Gradual fibrosis and atrophy of the thyroid parenchyma lead to a reduction in the size and volume of the thyroid gland. In clinical examinations, the thyroid gland in elderly individuals is often not palpable. Due to dietary restrictions on salt intake, elderly individuals receive less iodine through iodized salt.
Digestive problems and impaired absorption also contribute to reduced gastrointestinal iodine absorption. Thyroidal uptake of iodine in the bloodstream is also diminished in older adults. These changes result in decreased thyroxine (T4) hormone production.
However, despite the decline in T4-to-T3 conversion due to reduced deiodinase enzyme activity in older adults, blood levels of T4 remain within the normal range. T3 hormone levels may show a decrease. Thyroid-stimulating hormone (TSH), secreted by the pituitary gland, increases slightly with age. The natural reference range for TSH in individuals under 40 is between 0.4 and 5.4 milliunits per liter. After age 40, TSH gradually increases, adding approximately 0.3 milliunits per liter for each decade of age. Thus, after age 80, the maximum natural level of TSH is considered to be between 5 and 8 milliliters per liter.
Thyroid Diseases in the Elderly: Which Ones Are Common?
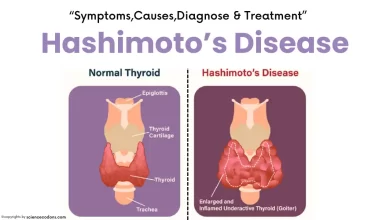
Thyroid diseases are not restricted by age and can occur at any stage of life. Generally, these diseases result from dysfunction of the thyroid gland (either hyperthyroidism or hypothyroidism), thyroid inflammation (thyroiditis), or thyroid tumors (benign nodules and cancers). The prevalence of thyroid tumors (both benign and malignant), hypothyroidism, and autoimmune thyroid diseases (such as Hashimoto’s thyroiditis) increases significantly with advanced age. In regions where iodine deficiency persists, goiters resulting from iodine deficiency can also be common among older adults. Fortunately, due to iodine deficiency control efforts in our country during recent decades, disorders related to iodine deficiency are rare in the Iranian population, especially among the elderly.
1- Hyperthyroidism (Thyrotoxicosis):
Hyperthyroidism occurs due to an excess of thyroid hormones circulating in the blood. The most common cause is an autoimmune disease called Graves’ disease. However, in older adults, multinodular goiters are more prevalent. Clinically overt hyperthyroidism affects less than 1% of individuals under 60 years old but increases to a maximum of 2% after the age of 60.
Subclinical hyperthyroidism (characterized by low TSH levels with normal thyroid hormone levels) is more common in older adults, affecting 3% to 8% of this population. The annual risk of progressing to overt hyperthyroidism in these individuals is approximately 1%. Elderly individuals are more sensitive to excess iodine intake, which can lead to a specific type of hyperthyroidism known as Jod-Basedow disease. The peak prevalence of hyperthyroidism occurs between the ages of 20 and 30, but 10% to 15% of hyperthyroid patients are over 60 years old.
Clinical Manifestations of Hyperthyroidism in the Elderly:
Thyroid overactivity (hyperthyroidism) in older adults presents differently from other age groups and can often be misleading. In elderly patients, the prominent signs of thyroid overactivity are observed in only about one-third of cases. The remaining patients may exhibit symptoms such as depression, chronic fatigue, altered cognition, apathy, weakness, muscle breakdown, weight loss, rapid thinning (which is sometimes mistaken for cancer), constipation (instead of diarrhea), reduced appetite (instead of increased hunger), fatigue, lethargy (instead of irritability), drooping eyelids (instead of eye protrusion), and absence of an enlarged thyroid (goiter). These atypical clinical features can confound the diagnosis of thyroid overactivity in older adults.
Some elderly patients with thyroid overactivity may experience restlessness and altered consciousness, a condition known as “thyrotoxic encephalopathy.” Thyroid overactivity also affects the cardiovascular system, leading to arrhythmias (including atrial fibrillation), chest pain, and congestive heart failure. We wrote a complete guide about Hyperthyroidism symptoms.
While eye manifestations of Graves’ disease (a common cause of hyperthyroidism) are less frequent in the elderly, they can be more severe when classic eye lesions are present. Generally, eye symptoms associated with Graves’ disease are more common in women and younger individuals but tend to be more severe and have worse outcomes in men and the elderly. Patients typically lack specific clinical signs of thyroid overactivity in clinical and subclinical hyperthyroidism (where TSH levels are below the lower limit of normal in the presence of normal thyroid hormone levels). The clinical significance of subclinical hyperthyroidism lies in its potential complications, including progression to overt clinical hyperthyroidism, atrial fibrillation, bone mass loss, and osteoporosis, especially in postmenopausal women. Neuropsychiatric manifestations are also relevant.
Diagnosis of Hyperthyroidism in adults:
Diagnosing thyroid overactivity (hyperthyroidism) in older adults differs from other age groups based on laboratory tests. When TSH decreases below the lower limit of the normal range, and T3 and T4 levels rise above the upper limit of normal for older age groups, it indicates clinical thyroid overactivity. Subclinical thyroid overactivity is considered if TSH is reduced while T3 and T4 remain within normal ranges.
Treatment of Hyperthyroidism in adults
In older adults, treatment for thyroid overactivity may involve methimazole (an antithyroid medication) or radioactive iodine therapy. Before administering radioactive iodine, patients should discontinue antithyroid drugs (such as methimazole) for several weeks. Over 80% of patients experience hypothyroidism (underactive thyroid) for weeks to months, necessitating lifelong thyroid hormone replacement. Surgical removal of the thyroid gland is not recommended due to non-thyroid-related conditions (such as heart and lung diseases) that increase surgical risks. However, if a large goiter causes compressive effects or if a patient has suspicious thyroid nodules, thyroid surgery is advisable.
2- Hypothyroidism in the Elderly
Hypothyroidism, or reduced production of thyroid hormones, is prevalent in elderly patients. Its symptoms are often nonspecific and can sometimes be mistaken for normal aging. Common manifestations of hypothyroidism in the elderly include:
- Fatigue
- General weakness
- Slowed mental function and cognitive impairment
- Sleepiness
- Feeling cold
- Dry skin
- Constipation
- Hearing impairment
In some cases, additional symptoms such as facial puffiness, muscle swelling, depression, decreased superficial sensation (paresthesia) and delayed deep reflexes aid in diagnosis. Notably, cardiac symptoms related to hypothyroidism are more common in the elderly than in other age groups. However, clinical examination alone identifies hypothyroidism in only 10% to 20% of elderly cases, emphasizing the importance of thyroid testing.
Diagnosis
Distinguishing hypothyroidism from normal aging, Parkinson’s disease, depression, or Alzheimer’s disease can be challenging. Key diagnostic tests include measuring serum levels of thyroid-stimulating hormone (TSH) and thyroxine (T4). In clinical hypothyroidism, TSH levels are elevated, and T4 levels are lower than the upper and lower limits of the normal range. Elevated TSH alongside normal T4 within the reference range confirms subclinical hypothyroidism.
Treatment
Most cases of hypothyroidism require lifelong treatment. The preferred therapy is levothyroxine, a synthetic thyroid hormone. In elderly patients with concurrent cardiovascular conditions, caution is necessary when prescribing levothyroxine due to potential risks. Typically, treatment starts with low doses (e.g., 25 micrograms per day) and gradually increases every 4 to 6 weeks until reaching the appropriate maintenance dose (usually around 100 micrograms per day).
Reference:
- https://www.ncbi.nlm.nih.gov/books/NBK555975/
- Mayo Clinic: https://www.mayoclinic.org/
- American Thyroid Association