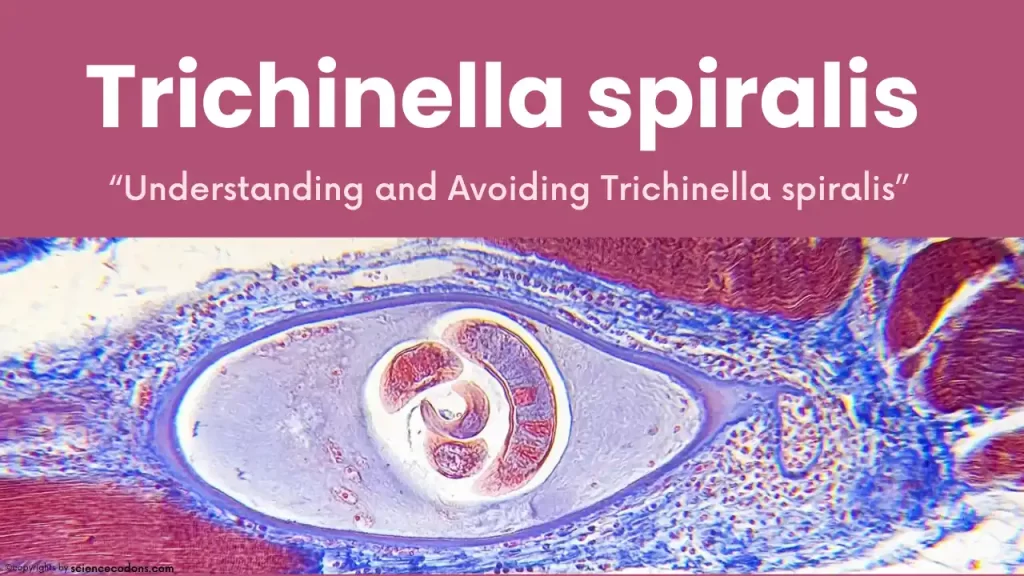
Trichinella spiralis is a type of worm that is responsible for causing the disease known as Trichinosis. This worm was first discovered by a medical student named James Paget in 1835. At the time, Paget was examining a corpse that had succumbed to tuberculosis. During this examination, he found larvae present in the body’s muscles. These larvae were later identified as Trichinella spiralis, confirming them as the cause of Trichinosis.
Unmasking the Characteristics of Trichinella spiralis
Trichinella spiralis is a type of worm that is found worldwide, particularly in countries where pigs are raised. This worm can infect multiple hosts and is commonly found in animals. When a parasite has various animal hosts, the condition is called ‘Enzootic.’ To date, 11 species of Trichinella spiralis have been identified. In Iran, there has been one case of a person testing positive for this parasite.
Trichinella spiralis is white in color. The anterior part of the worm, which is its head, is typically thin. One-third of the worm’s body length comprises its intestine, which is bead-like or ‘Stichocytes‘ in structure. Rodents are the primary hosts for Trichinella spiralis, but they can also serve as intermediate hosts, a condition known as ‘Autoheteroxen.’
Female Trichinella spiralis worms measure 3-4 millimeters in size. They have a single-chambered uterus, known as ‘Monodelphic,’ and can produce larvae. These larvae are approximately 100 microns in size and are severely twisted, hence the name ‘spiralis‘ or spring-like. The genital opening of the worm is located at the anterior part, while the uterus and ovary are typically situated at the posterior part.
Male Trichinella spiralis worms are smaller, measuring 1.5 millimeters in size. The end of these worms is usually slightly curved. They possess a spring-like auxiliary mating organ known as the ‘testicule‘ and have two ‘papillae,’ distinguishing morphological features of this male worm.
Note: The ovary is behind, and the female is bigger than the male.
Life Cycle of Trichinella spiralis
The life cycle of Trichinella spiralis is categorized into two stages: the domestic cycle and the wild cycle. This worm has multiple hosts and is prevalent among animals, leading to a condition known as ‘Enzootic.’
Domestic Cycle
In the domestic cycle, the life cycle involves pigs, wild boars, and rodents. These animals can serve both as the final and intermediate hosts. They can consume each other’s meat or leave their meat products and waste for pigs that are infected with the worm, thereby spreading the infection.
Wild Cycle
In the wild cycle, the infection can be transmitted among different prey and predators. Humans are considered a biological dead-end for this worm because human meat is not typically consumed by any other creature unless in rare instances where a human is hunted and consumed by a predator.
Infection with Trichinella spiralis in humans usually occurs through the consumption of meat from pigs or game animals that are infected with larvae. The meat is digested, releasing the larvae in the intestine, which mature within two days. After maturing, the larvae mate, and the female worms begin to lay larvae in the intestinal villi. These larvae then enter the bloodstream. Larviposition usually continues for 4-14 weeks in female worms. 1-2 weeks after consuming infected meat, larvae can be observed in the bloodstream.
After this period, the larvae of Trichinella spiralis migrate to various muscles, including the diaphragm, tongue, throat, abdomen, intercostal muscles, deltoid muscles, and breasts. Here, the larvae are encapsulated three weeks after infection. Approximately 6-12 months after the larvae have encapsulated, calcification of the larvae occurs, leading to the manifestation of symptoms and the eventual death of the larvae in these muscles.
Symptoms of Infection with Trichinella spiralis(Trichinosis)
The symptoms of Trichinella spiralis infection are categorized into three stages based on the location of the worm in the body: Invasion, Migration, and Encystation.
During the Invasion stage, which takes place in the intestine, symptoms typically persist for 2 to 3 days. These symptoms include nausea, fever, abdominal pain, diarrhea, headache, and dysentery.
The Migration stage usually occurs in the bloodstream. Symptoms during this stage last for 1-2 weeks and include edema, conjunctivitis, fever, chills, sweating, photophobia (light sensitivity), muscle pain, and severe eosinophilia, which can reach up to 90%.
The Encystation stage involves extreme weakness and weight loss (Cachexia), swelling of the hands and feet, low blood pressure, heart muscle involvement leading to chest pain, tachycardia (increased heart rate), and intravascular clotting. This clotting can lead to a stroke and potentially result in the patient’s death.
If the brain is affected, symptoms can include headache, delirium, numbness, granuloma in the brain, coma, loss of natural body reflexes, meningitis, and encephalitis. These symptoms can ultimately lead to the patient’s death in 5 to 6 percent of cases.
Symptoms of Trichinosis:
- Initial Signs and Symptoms (1 to 2 days after infection):
- Diarrhea
- Stomach (abdominal) pain
- Severe tiredness and weakness (fatigue)
- Nausea and vomiting
- Later Signs and Symptoms (about a week after infection):
- High fever and chills
- Muscle pain and tenderness
- Aching joints
- Swelling of the eyelids or face
- Weakness
- Headache
- Sensitivity to light
- Pink eye (conjunctivitis)
| Stage | Symptoms |
|---|---|
| Initial | Diarrhea, Abdominal pain, Fatigue, Nausea, Vomiting |
| Later | Fever, Muscle pain, Joint pain, Swelling, Weakness, Headache, Sensitivity to light, Pink eye |
Eat Smart, Stay Safe: Your Guide to Preventing Trichinellosis
Preventing Trichinella Spiralis infection involves avoiding or reducing exposure to raw or undercooked meat containing the parasite. The prevention measures include:
- Cook meat thoroughly until the internal temperature reaches at least 71°C (160°F) for pork and 77°C (170°F) for wild game. Cooking can kill the larvae and make the meat safe to eat.
- Freeze meat for at least 20 days at -15 °C (5°F) or for at least 10 days at 23°C (- 10°F). Freezing can kill most of the larvae, except for some freeze-resistant species, such as T. nativa or T. britovi.
- Curing, smoking, drying, or salting meat for at least 30 days. These methods can kill some of the larvae but are unreliable and should not be used alone.
- Avoid eating raw or undercooked meat, especially pork, horsemeat, or wild game. This includes avoiding eating meat products, such as sausages or ham, that are not adequately cooked or processed.
- Avoid cross-contamination of cooked and raw meat by using separate utensils, cutting boards, and plates and by washing hands and surfaces after handling raw meat.
- Controlling the infection in animals by preventing them from eating raw meat or carcasses containing the parasite and testing them for the disease before slaughter.
Diagnosis and Treatment of Trichinellosis
The symptoms of the disease are instrumental in its diagnosis. A history of consuming raw pork can also be a significant indicator. Patients typically experience pinpoint bleeding under the nails and general discomfort or malaise. Severe eosinophilia, a condition where there is an abnormally high number of eosinophils (a type of white blood cell) in the body, is a strong indicator of Trichinella infection (eosinophilia can range from 50-90%). A definitive diagnosis is made through a muscle biopsy and the observation of twisted, spring-like larvae. Serological tests such as ELISA and Immunoelectrophoresis can also assist in the diagnosis by detecting antibodies against antigens of Trichinella spiralis.
For prevention, one strategy could be to treat pigs, as eliminating the infection in pigs removes the source of infection. It is also recommended to cook and freeze pork, which can kill the worm in the meat and prevent its transmission to humans.
treatment
To treat and reduce the inflammatory response to larvae encapsulated in the muscles, ‘corticosteroids’ can be used, typically prescribed at 40-60 milligrams daily. For treating adult worms, Mebendazole can be used; a dosage of 200 milligrams daily for 5 days is usually sufficient. Also, Albendazole (400 milligrams daily for 2 days) and Pyrantel Pamoate (10mg/kg daily for 5 days) are used to treat adult worms. It’s important to note that the use of these drugs should be under the supervision of a doctor, and self-medication should be avoided.
Conclusion
Trichinella Spiralis is a roundworm that can infect humans and animals by living in their muscles. It is the cause of a disease called Trichinosis, which can cause severe complications if not treated. Trichinella Spiralis is transmitted by eating raw or undercooked meat that contains the worm larvae. The symptoms and complications of Trichinella Spiralis infection depend on the stage, severity, and duration of the infection, as well as the host’s immune response and general health. The diagnosis of Trichinella Spiralis infection is based on the clinical symptoms, the history of exposure to raw or undercooked meat, and the laboratory tests. The treatment of Trichinella Spiralis infection involves medication and supportive care. Preventing Trichinella Spiralis infection consists of avoiding or reducing exposure to raw or undercooked meat containing the parasite.
Reference:
- Trichinellosis | SpringerLink
- https://www.cdc.gov/dpdx/trichinellosis/
- https://doi.org/10.4269%2Fajtmh.1977.26.68
- EXPERIMENTAL TRICHINIASIS – PubMed (nih.gov)
- The draft genome of the parasitic nematode Trichinella spiralis | Nature Genetics